Ilana Katz MS, RD, CSSD
Hyponatremia tends to be mostly associated with athletes who participate in long duration sports such as marathons and triathlons. Endurance athletes taking in water during training or an event can develop hyponatremia, a potentially life threatening condition that occurs when sodium levels drop to a dangerous low in the blood stream (below 135 mmol/L (of blood). Early symptoms may include nausea, drowsiness, confusion, headache and fatigue. These can quickly progress to seizures, coma and death if not resolved in time. Importantly, athletes are not the only population that needs to be aware of this deadly phenomenon.
Dilution of sodium can result, as mentioned, from over-drinking, but also from water retention (often a side effect of various medications). Sodium can be lost in various ways other than dilution which include urination, perspiration and gastrointestinal distress (vomiting/diarrhea). Furthermore certain medical conditions such as congestive disease, kidney dysfunction and ineffective ant-diuretic hormones are known causes.
Since hyponatremia has usually been associated with endurance sports, those who engage are much more well-informed than in the past, and emergency staff who treat athletic stress conditions are also far better educated to recognize and manage symptoms, and even play a role in prevention. The sports medicine community has been helpful in raising awareness about risks and signs of over-hydration. However, with obvious evidence that there are many other populations at risk for hyponatremia, it is vital to recognize these so that all health care professionals are on the leading edge of avoidance and if necessary, acute care.
Some examples of patients who may be eligible for high alert:
- Psychiatric patients with a syndrome known as psychogenic polydipsia, meaning they drink excessive amounts of water..
- Multi-pharmocological patients (especially elderly). Why, well because many medications have potential risks.
- Diuretics deplete electrolytes, including sodium
- Antidepressants increase level of antidiuretic hormone
- Patients being administered intravenous hypotonic fluids: hypotonic fluids contain a lower concentration of sodium than blood and thus excessive quantities at high entry rate can dilute sodium.
- Tube fed patients: proper fluid levels and electrolyte balance must be continuously monitored and orders adjusted based on results of consistent blood work.
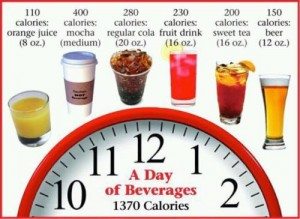
There is also the all controversial sodium debate to consider. Researchers and health practitioners often have opposing arguments as to whether dietary sodium should always be strictly conserved. While lowering sodium is unarguably beneficial for those already diagnosed with hypertension (high blood pressure), increasingly conservative recommendations for the average population is often contested. The argument being that too little sodium can lead to other health problems, the main one being hyponatremia. Interestingly, the dietetic community are in agreement that avoidance of dietary sodium is unlikely to cause hyponatremia. Even a very low sodium diet of 500 – 1000 mg/day should maintain adequate levels under normal circumstances. It is the complexity of what defines “normal circumstances.”
In summary, with regards to controlling appropriate levels of sodium in the blood and avoidance of hyponatremia, not only athletes should be aware of hyponatremic signs and symptoms. For those with a normal blood pressure, eating patterns and water intake should be developed based on clinical judgement, guidelines and scientific evidence.